Imagine a metal, scaffold-shaped implant that could support the regrowth of a shattered bone. All that would be needed would be an initial CT scan, a virtual construction of the implant and a metal printer to produce the final product. Devastating outcomes like amputation or loss of the ability to walk could be prevented.
While this type of innovation may seem outside the realm of modern technology, several Duke professors have made such futuristic biomaterial implants a reality, including Ken Gall, professor in the department of mechanical engineering and materials science; Shyni Varghese, professor of orthopaedic surgery and Matthew Becker, Hugo L. Blomquist distinguished professor of chemistry.
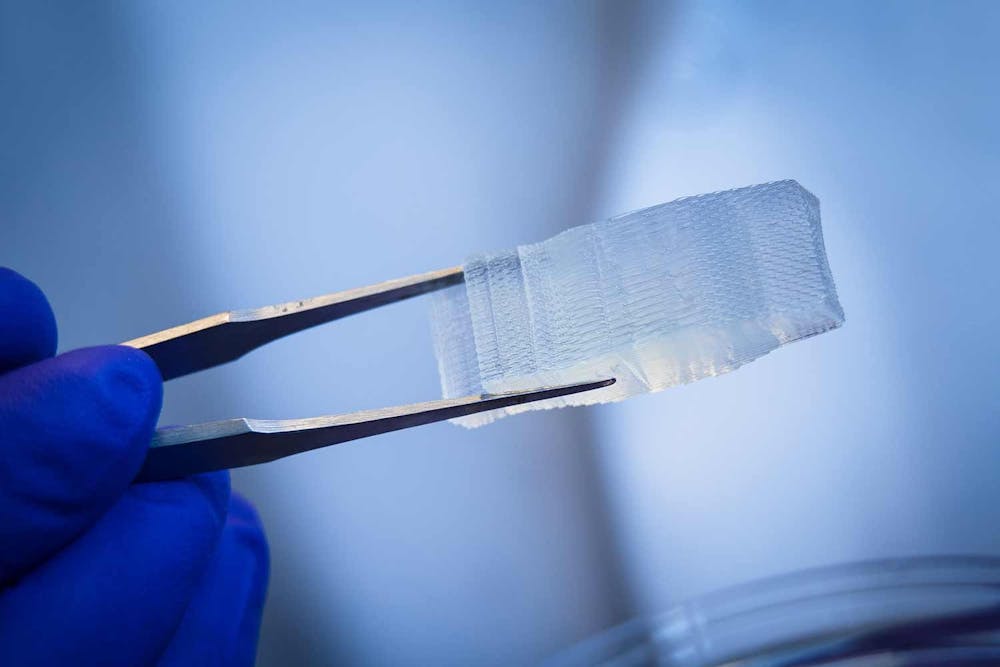
Gall’s research focuses on the use of 3D printed metals and polymers, including the aforementioned metal scaffold, using synthetic hydrogels for cartilage replacement and other related explorations. He also has initiated a new project investigating the types of structures that can be printed and is looking into utilizing machine learning or other algorithms to predict how these structures will behave.
While Gall’s research spans a large breadth of biomaterials, the common link among these implants is their ability to perform some structural function, he said.
“We try to figure out how [to] make these materials integrate with the body so they survive there,” Gall said. “Our approach has always been [to] put something in that is actually better than what you started with.”
Varghese’s research focuses more specifically on the utilization of the biomolecule adenosine to promote bone formation and prevent bone degeneration. She has developed three implants that could utilize adenosine to promote fracture healing, the first of which takes advantage of the nanomolar amounts of adenosine already existing in the body.
While normal adenosine levels are usually too low to promote healing, cells under stress during an injury secrete more of the molecule. Hence, Varghese proposed a biomaterial implant that can sequester this released adenosine during cell stress and ensure it stays in the body for a longer time to promote healing.
Adenosine levels decrease in the case of a disease. To address insufficient levels of the biomolecule in patients, Varghese created an implant that delivers additional adenosine to the body.
Outside of adenosine, Varghese’s lab has been investigating self-repairing lubricants for joint injuries and potentially even dry eyes. She is also working on a nanocarrier drug implant that can be administered orally to treat bone loss caused by osteoporosis.
Becker’s research aims to “bring new material, fundamental building blocks, into the realm of possibility,” he said. He hopes to use these new biomaterials to fulfill unmet medical needs and material challenges across a variety of medical disciplines.
One of the implants that Becker has developed consists of a degradable polymer film made of amino acid-based polyester ureas loaded with analgesics. The film can be implanted after laparoscopic surgery or a C-section and can control pain locally for four to five days. This would mean that opioid pain relief medication would no longer be needed for patients post-surgery.
“It’s my hope that before I’m done with this … that one of the polymers developed in my lab actually makes it to a patient. And it looks like we’re getting close,” Becker said.
One of Becker’s favorite memories in the lab involved working with the Department of Defense to develop degradable plastic polymers for soldiers injured by improvised explosive devices or gunshot wounds. The polymers would fill two to three inches of bone lost during the injury and salvage the limb, avoiding the need for amputation. Becker’s lab tested the efficacy of the polymer in a sheep model. After four hours after surgery, the sheep was able to stand up and walk.
“That was probably my most memorable ‘wow’ moment simply because we had no idea if it would work,” Becker said.
Varghese’s favorite memory in her lab was working on soft robotics with one of her graduate students. Varghese asked the graduate student to see if they could use the self-healing gel in the lab to produce a soft robot, and a few months later, the student was able to make Varghese’s vision a reality.
“Giving some vague, imaginary, dreamy ideas to the students and then working with them and figuring out those things has always been fun,” Varghese said.
Gall’s favorite part of his work is watching the biomaterials discovered in his lab eventually become implanted in a person.
“It’s exciting to be able to say that we published the first paper that showed this. And then the first patients that ever had this in their body, we helped that happen,” Gall said.
Get The Chronicle straight to your inbox
Signup for our weekly newsletter. Cancel at any time.
Ayra Charania is a Trinity junior and a senior editor of The Chronicle's 118th volume.