When a peanut is enough to trigger anaphylactic shock in some people, allergies are not just life-threatening, they’re life-altering—people live in constant fear that if they're not careful, any exposure could kill them.
That’s why scientists at Duke Health researched the mechanism by which immune cells are activated during anaphylactic shock. Before this study, scientists knew that mast cells released substances that can cause anaphylaxis when allergens entered the blood steam. But since mast cells cannot penetrate blood vessel lining, scientists were unsure how mast cells would know that allergens were in the blood stream.
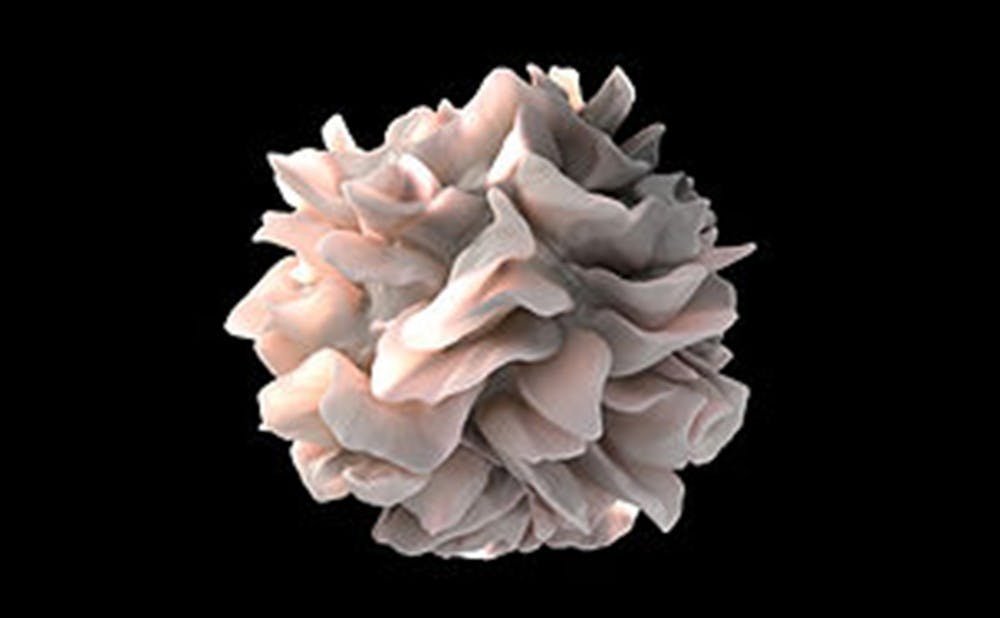
The team's work, published in the Nov. 9 issue of the journal Science, used mice models to discover that immune cells—dendritic cells—establish the contact between mast cells and allergens, sending the body into shutdown mode. With this discovery, new approaches can be developed to tackle deadly anaphylaxis.
“We found that the dendritic cells play a direct role in anaphylactic shock, which opens up huge possibilities for future medicine,” said Hae-Woong Choi, lead author and researcher in Duke's Department of Pathology.
Allergies occur when the body mistakenly deems a substance harmful, causing mast cells to release mediators that cause symptoms such as watery eyes and a runny nose. Anaphylaxis is more dangerous than a regular allergy response, and can cause difficulty breathing, lowered blood pressure and death.
Although we understand the effects of anaphylactic shock, we don’t have a strong understanding of how it takes place or why it occurs so quickly.
Through altering the levels of immune cells in mice and then injecting them with toxins, researchers noted how these levels affect the intensity of anaphylactic shock.
When dendritic cells were lowered or removed, the mice experienced no anaphylactic symptoms. The researchers discovered how dendritic cells used probe-like dendrites to quickly penetrate blood vessel walls, access allergens in the blood, and pass them along to mast cells. The mast cells then churned out mediators that cause anaphylactic symptoms.
So, without dendritic cells, mast cells would never be able to access the allergens, and anaphylaxis would not occur, according to this research.
It is well-known that in a typical immune response, these dendritic cells usually internalize and process allergens before presenting them to mast cells. But, especially in the case of anaphylaxis, the process is much faster.
“Dendritic cells now appear to actively distribute allergens they have acquired to surrounding immune cells even before they are internalized,” Choi said, explaining why the body can have such a strong response in mere seconds.
Since this discovery is so recent, nothing concrete can be said about the future of anaphylaxis prevention.
Current drugs focus on neutralizing the mediators released by mast cells and blocking symptoms from manifesting. Now, the researchers believe this finding changes the strategy for combating anaphylactic response by targeting dendritic cells. It’s not as easy as limiting dendritic cell ability, however, since they may play a role in regular immune response as well.
"Maybe these dendritic cells are designed to detect blood-borne parasites, viruses or bacteria, so we need to understand any other circumstances that activate them before contemplating shutting them down or impeding their activity," said senior author Soman N. Abraham, professor in Duke's Departments of Pathology, Immunology and Molecular Genetics & Microbiology, in a news release.
Get The Chronicle straight to your inbox
Sign up for our weekly newsletter. Cancel at any time.